Objective
To determine the effectiveness of MANUAL’s medically supervised digital lifestyle programme on weight loss.
Introduction
What is obesity? What are its causes?
Obesity is defined as a person having an abnormal or excessive accumulation of fat, with categories ranging from overweight (BMI 25.0 to < 30 kg/m²) to obese (BMI > 30 kg/m²)1.
The fundamental cause of overweight and obesity is an energy imbalance between calories consumed and calories expended. Globally, there have been:
- An increased intake of energy-dense foods that are high in fat and sugars (e.g. junk food)
- An increase in physical inactivity due to the increasingly sedentary nature of many forms of work, changing modes of transportation and increasing urbanisation
Additional factors that contribute to overweight/obesity include genetics, comorbidities (i.e. PCOS in women, hypogonadism, hypothyroidism, etc.) medication use (antidepressants, local corticosteroids, insulin, etc.), mental health disorders (eating disorders and depression), and lifestyle (alcohol abuse, yo-yo dieting, obstructive sleep apnea, stress, etc.).
Delve deeper into possible reasons why you’re not losing weight here.
Discover foods that help weight loss here.
For tips on losing weight without exercise, learn about it here.
Why is this something I need to care about??
In 2022, the majority of adults (64%) were estimated to be overweight or obese. Globally, obesity is projected to impact over 4 billion people by 2035.
This is troubling because obesity is a complex disease that is a significant risk factor for chronic diseases1 2 3 that can seriously impact quality of life and life expectancy4.
If you are struggling to keep motivation for losing weight, click here.
Does current research shed any light on this increase?
While the initial approach to managing obesity includes suggesting lifestyle changes in diet, physical activity, and more general lifestyle, studies have revealed that interventions focusing solely on caloric deficit and increased physical activity have limitations in sustaining long-term weight loss5
Professional organisations now recommend anti-obesity medications for individuals who have insufficient results from lifestyle treatment alone, while emphasising that these medications are based on the individual needs of the patient 6 7 8. Among these medications, Glucagon-like Peptide-1 receptor agonists (GLP-1s), which have been traditionally used for type 2 diabetes9, have shown promise in obesity prevention and treatment10 11 12 13.
How do the GLP-1s work?
GLP-1s help regulate hunger by imitating your appetite hormone, medically known as the GLP-1 hormone. This imitation results in a delay in your stomach emptying which means you feel satiated and full for longer. Ultimately, this process helps in reducing food intake and promoting weight loss.
When combined with lifestyle interventions, these medications can lead to a significant reduction in total body weight. While GLP-1s offer a bridge between traditional weight loss methods and more invasive interventions, they are still fairly new in terms of this use case, so their long-term efficacy and impact beyond six months are areas still under exploration.
Find out more about GLP-1s here, including its benefits and side effects.
What is the evidence gap?
Despite these advancements, only a small percentage (1-2%) of eligible adults receive prescriptions for obesity medications, and even fewer integrate them into intensive lifestyle modification programmes14.
This means there is a critical need for a more integrated and comprehensive healthcare approach and research to address the barriers hindering the adoption of effective programmes that combine these pharmacological solutions with behavioural and lifestyle modifications, to bring down levels of obesity in adults.
At MANUAL, we have developed a medically supervised digital behavioural change programme to investigate the impact of the 6-month programme on weight and BMI among adults with overweight and obesity.
Methods
In March 2024, we conducted a (retrospective observational single-cohort) study of 439 customers aged 19-83 years old who completed at least 1 coaching session.
Eligibility
Potential candidates completed (in the following order):
- A medical questionnaire, including reasons for wanting to start treatment
- A weight submission (via photo and input)
Inclusion:
- BMI above 30 kg/m2
- BMI above 27 kg/m2, with additional comorbidities
What happened next?
Eligible patients received an informative video consultation with our in-house clinicians who specialise in GLP-1 treatment.
After patients provided consent to receive treatment, clinicians prescribed the appropriate GLP-1 treatment based on the individual’s needs and goals.
Treatment options included:
- Ozempic, Wegovy, or Rybelsus (active ingredient: Semaglutide)
- Saxenda, Victoza (active ingredient: Liraglutide)
- Trulicity (active ingredient: Dulaglutide)
- Alli, Orlos (active ingredient: Orlistat)
- Mounjaro (active ingredient: Tirzepatide)
How was progress recorded?:
We did a follow-up with each patient every 3 months after starting treatment. At each time point, patients uploaded photos of their weight (measured via scale). Patients had unlimited access to medication management support from clinicians to ensure the safety of treatments (including dosage adjustments) and to manage any side effects. Patients also received resources for healthy recipes and workout plans and also had the option to engage in biweekly 1:1 coaching calls with registered nutritionists and psychologists for coaching advice to discuss anything from goal setting and emotional eating, to navigating relapses/failure and progress tracking, etc.
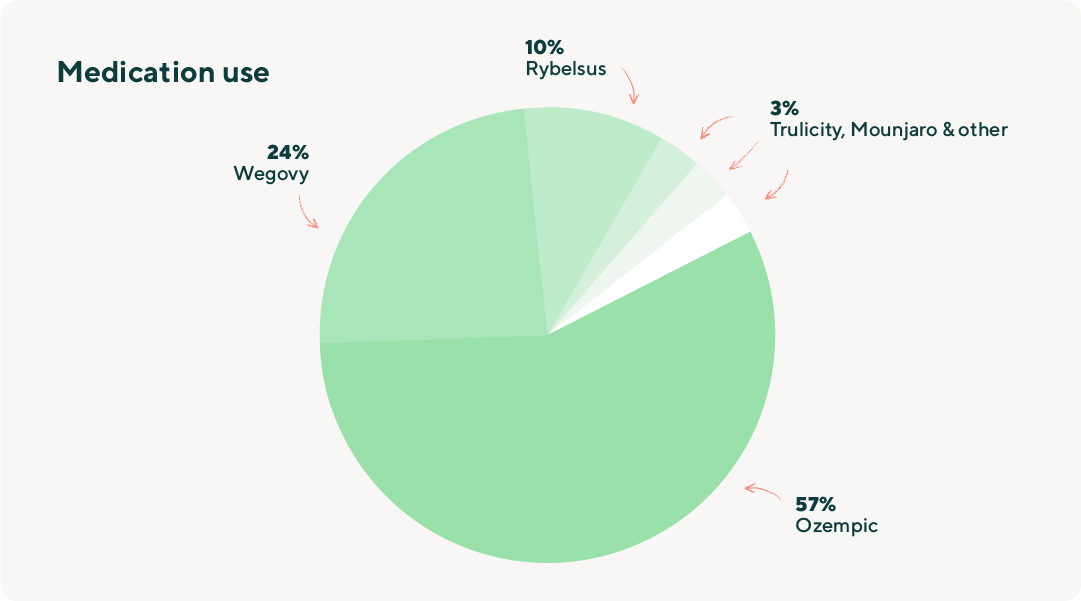
Medication Use
The proportion of patients on the various medications were as follows: 57% on Ozempic, 24% on Wegovy, 10% on Rybelsus, 3% on Saxenda, 3% on Trulicity, 3% on Mounjaro, Victoza, Alli, or Orlos.
Results
Baseline summary statistics were summarised by means and standard deviation (SD). Respondents were categorised by age, gender, BMI, and medication type.
Among the patients eligible for 6 months of observation (N=439), their mean BMI at baseline was 35.8 (SD 6.2), with 92% reporting as obese, and 8% as overweight. The mean age was 44.4 (SD 11.3). 77% reported as female, 33% with hypertension, 22% with cholesterolemia, 12% with type 2 diabetes.
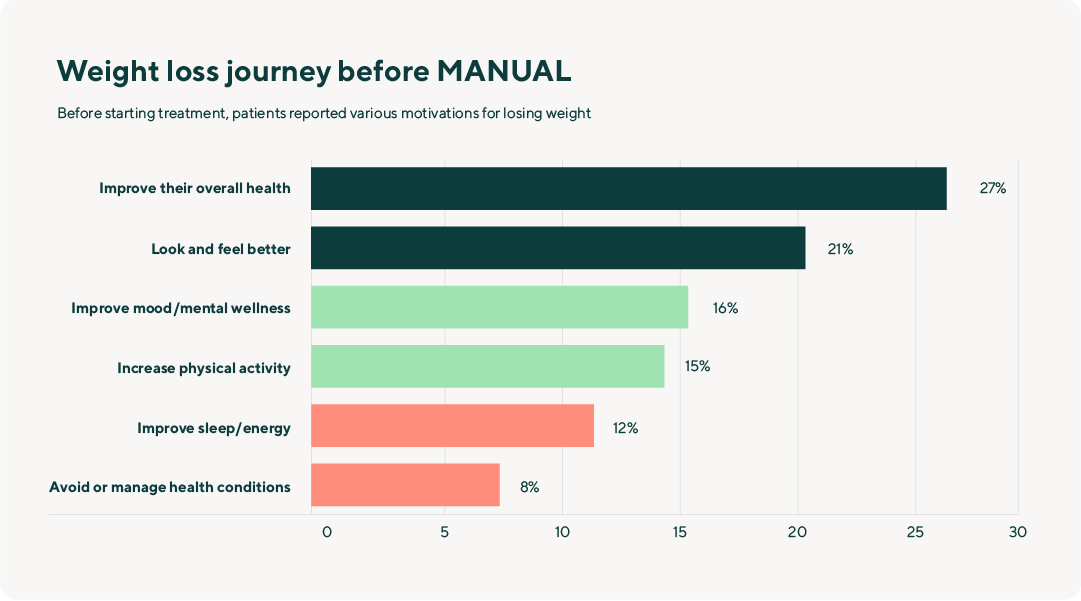
Respondents’ Weight Loss Journey Before MANUAL
Before starting treatment, patients reported various motivations for losing weight: 27% of patients expressed a desire to improve their overall health, 21% aimed to look and feel better, 16% sought to improve their mood or mental wellness, 15% aspired to increase their physical activity, 12% targeted improved sleep or energy levels, and 8% strived to avoid or manage health conditions.
The majority of patients (94%) reported prolonged struggle with weight-related challenges over their lifetime: 45% of patients with their entire life, 19% in the last 10 years, and 30% in the past 5 years.
Before starting with MANUAL, 22% had experimented with dieting, 21% increased their exercise regimen, 19% engaged in calorie-counting, and 9-14% had explored weight loss programmes, meal replacements, and/or weight loss supplements.
The most common challenges patients faced when changing their eating habits included food cravings (22%), persistent hunger (21%), stress-induced eating (19%), frequent snacking (18%), and swinging between disciplined eating and binge eating (17%).
The most prevalent challenges reported with exercising/staying more active were loss of motivation (32%), time constraints (20%), discomfort exercising in public (17%), complications from injury/illnesses (14%), and lack of enjoyment in exercise (12%).
The biggest challenges to maintaining weight loss progress were issues in consistency (32%), loss of motivation (29%), yo-yo weight fluctuations (26%), and time constraints (11%).
MANUAL Program Effectiveness
After 6 months, patients (N=439) experienced a statistically significant (p<0.01) weight reduction of 10 kilograms (kg) (10% of their body weight) and BMI by 3.8 (6-month mean BMI: 32).
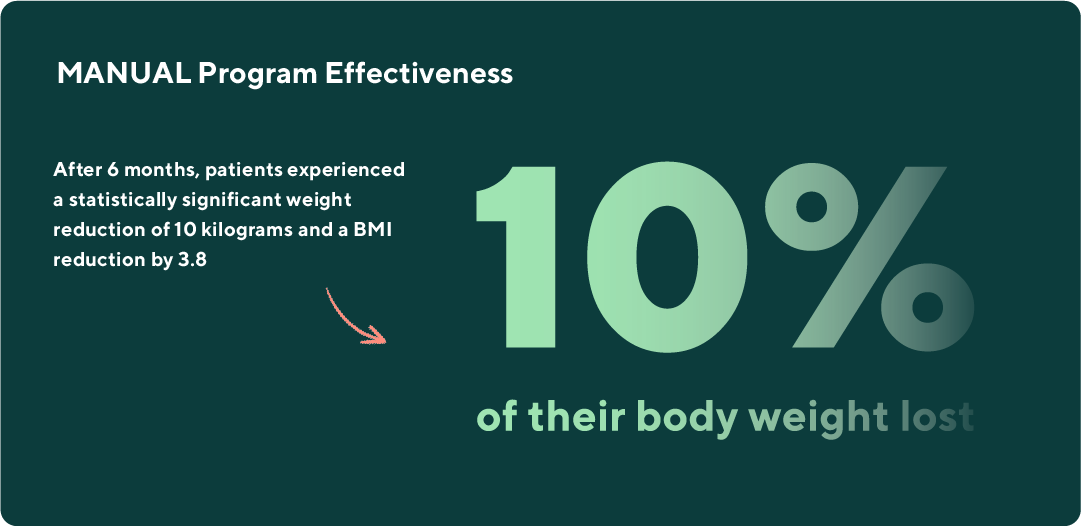
When categorised by medication, patients taking Rybelsus, Wegovy, and Ozempic experienced nearly identical reductions in their body weight (>10%) at the 6-month timepoint relative to their baseline weights. Observations were similar among individuals with obesity (BMI>30) and age subgroups (aged 25-34, 35-44, 45-65, 55+), and gender at birth (male, female). All results were statistically significant (p<0.05).
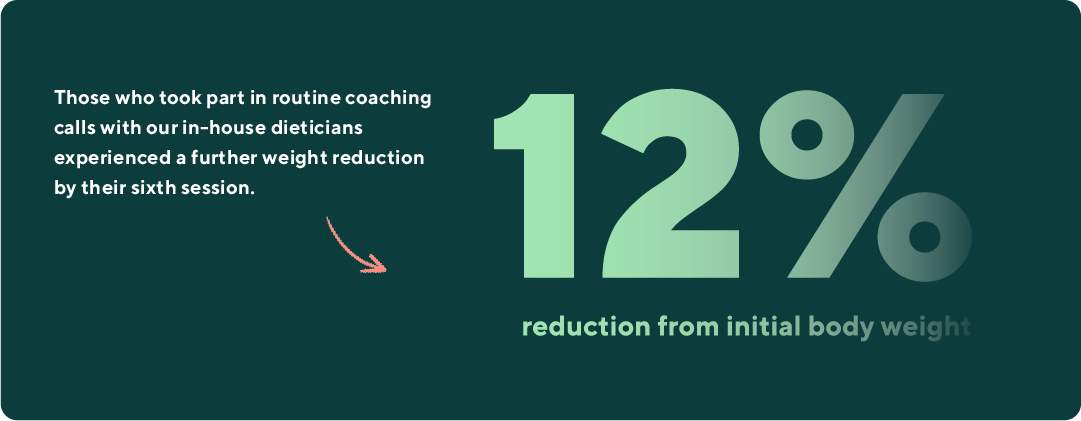
We found that those who took part in routine coaching calls with our in-house dieticians experienced a further weight reduction by their sixth session (12% reduction from initial body weight at baseline) compared to those who attended a single call, and continued to sustain their weight loss (even among those who completed 16 or more sessions).
Summary
The primary motivation for patients seeking weight loss treatment was to improve their overall health (27%), with the majority (94%) having struggled with weight issues throughout their life. Before using MANUAL, 22% of patients had tried other dieting methods, and the most common obstacles in changing eating habits and exercising were food cravings (22%) and loss of motivation (32%).
However, as individuals enrolled in the programme, they experienced improvements in their weight (-10%) and BMI (-3.8) over the span of 6 months. These observed changes remained consistent by gender, age, and BMI subgroups, highlighting the broad success of these treatments across diverse patient profiles. Notably, those who attended more coaching sessions experienced even more substantial reductions in weight (-12%) by the 6-month assessment point.
Discussion
The MANUAL programme, incorporating medication and lifestyle/behavioural treatment, has made a significant impact on participant weight loss, despite the psychological and psychosocial barriers that patients presented before treatment.
Patients who attended coaching sessions experienced a greater impact on their weight change, suggesting that the coaching enhanced both the short-term effectiveness and longer-term sustainability of weight management. Due to the complex and individual nature of obesity and weight loss, coaching sessions may offer a tailored and comprehensive approach (integrating behavioural, educational, and psychological components) to address each individual’s key challenges and needs through increased support and lifestyle changes to sustain their weight loss over time.
These results are ongoing; future analyses will evaluate change in weight at 12 months and subsequent time points to assess long-term efficacy. Cohorts will also receive validated quality-of-life questionnaires to comprehensively assess change in psychological and psychosocial domains. Future research is also needed to study different populations on a larger scale. These insights will play a pivotal role in informing clinician decision-making and guidelines for personalised treatment strategies, ultimately enhancing the overall effectiveness of therapeutic interventions with a focus on patient-centred care.
We will be conducting further research in collaboration with top Universities in the UK. If you are interested in participating and gaining early access to findings, please sign up here: research@manual.co. Your involvement could be a vital part of shaping the trajectory of obesity research. We value your potential contribution to fostering positive developments in overall well-being.
While we've ensured that everything you read on the Health Centre is medically reviewed and approved, information presented here is not intended to be a substitute for professional medical advice, diagnosis, or treatment. It should never be relied upon for specific medical advice. If you have any questions or concerns, please talk to your doctor.



